Leg Swelling & Iliac Vein Compression: What You Need to Know
Have you ever wondered why one leg swells more than the other? Or why you have leg pain that doctors can’t seem to explain? You might have something called iliac vein compression – and you’re definitely not alone.
What Is Iliac Vein Compression?
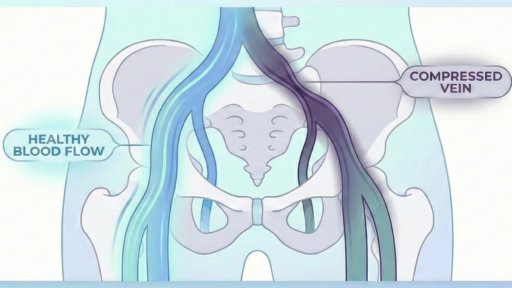
Think of your veins like garden hoses carrying blood back to your heart. Now imagine someone stepping on that hose from the outside. That’s basically what happens with iliac vein compression.
Your iliac vein is a major blood vessel in your pelvis that drains blood from your leg back to your heart. Sometimes, nearby arteries and your spine can squeeze this vein, making it harder for blood to flow properly. Doctors used to call this “May-Thurner syndrome”, today we refer to this as Pelvic Venous Disorder, but now we know it’s much more common than we once thought.
How Common Is Iliac Vein Compression?
Here’s something that might surprise you: up to 70% of peoplehave some degree of vein compression when doctors look at CT scans. But here’s the key – most of these people don’t have any symptoms at all!
However, if you have advanced leg problems like ulcers or serious skin changes, there’s about a 40-50% chance you might have significant vein compression that needs treatment.
What Symptoms Should You Watch For?
Not everyone with vein compression needs treatment. But you should talk to your doctor if you have:
- Swelling in one leg more than the other that really bothers you
- Chronic pelvic pain (especially in women)
- Leg ulcers or serious skin changes that won’t heal
- Symptoms that significantly impact your daily life
Remember: just because a test shows compression doesn’t mean you need treatment. Your symptoms matter more than what shows up on a scan.
How Do Doctors Diagnose Iliac Vein Compression?
Your doctor has several tools to figure out if vein compression is causing your problems. We recently wrote a paper on this topic. Here are the most common tests:
Duplex Ultrasound
This is usually the first test. It’s like getting an ultrasound during pregnancy – completely painless. The sonographer (a healthcare professional who specializes in the use of ultrasonic imaging devices) can see how blood flows through your veins and spot any blockages.
CT or MRI Scans
These give detailed pictures of your veins and surrounding structures. However, they only show you lying flat, which might not tell the whole story.
The Dynamic Test
Here’s something interesting: some compressions only happen when you’re lying down. When you stand up or turn on your side, the compression might disappear completely.
When Do You Need Treatment?
This is where it gets tricky. Not everyone with vein compression needs a stent (a tiny metal tube that opens up the vein). Treatment makes sense when:
- Your symptoms seriously affect your quality of life
- You have leg ulcers or severe skin changes
- Other causes have been ruled out
- Conservative treatments haven’t helped
Treatment is NOT recommended if your symptoms are mild or if there are other medical problems causing your leg issues that haven’t been addressed first.
The Bottom Line
If you have leg swelling, pain, or skin changes, don’t ignore them. But also don’t panic if a test shows vein compression. The most important thing is whether your symptoms are affecting your life.
Work with a doctor who:
- Takes time to understand your symptoms
- Considers your quality of life
- Explains why treatment is or isn’t right for you
Questions to Ask Your Doctor
- “Are my symptoms severe enough to warrant treatment?”
- “Have other causes of my leg problems been ruled out?”
- “What would happen if we wait and see?”
- “How much experience do you have with this condition?”
Remember, you’re not just a scan result – you’re a person with symptoms that matter. The best treatment decisions consider both what tests show ANDhow you feel.