What is Post-Thrombotic Syndrome (PTS)?
Ever wonder what happens after a deep vein thrombosis (DVT), or blood clot, clears up? For some people, the problem doesn’t end there. Enter Post-Thrombotic Syndrome (PTS)—a condition that can pop up after the clot has gone but leaves lasting damage to your veins.
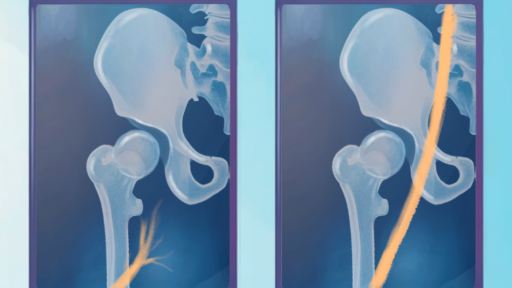
PTS is caused when a clot injures the valves in your veins, making it harder for blood to flow properly. Instead of moving smoothly through your veins, blood pools in your legs, leading to swelling, discomfort, and skin changes. Let’s dive into what this means for you and how to handle it!
How Do I Know If I Have PTS?
Here are some signs to look out for:
- Swelling in the affected leg (especially by the ankle)
- Pain or heaviness that gets worse after standing for a long time
- Skin discoloration or thickening
- Itchy skin or leg ulcers
How is Post-Thrombotic Venous Occlusion Diagnosed?
When diagnosing this condition, your doctor may start with an ultrasound to check the veins in your leg. Other imaging tests, like a CT scan or MRI, may also be used to get a better look at your veins and see where blood flow is blocked.
Getting accurate images is key because your doctor needs to understand the exact location and severity of the blockage to plan the best treatment.
Treatment Options for Post-Thrombotic Venous Occlusion
If you’re diagnosed with post-thrombotic venous occlusion, don’t worry—there are several effective treatment options. Here’s a look at the most common ones:
1. Stenting
- What It Is: A small, mesh-like tube called a stent is placed in your vein to hold it open and improve blood flow.
- How It Works: During the procedure, the doctor makes a small incision, guides the stent into the blocked vein, and expands it. This helps keep the vein open.
- Benefits: Stenting can reduce swelling, relieve pain, and improve your ability to walk and stand comfortably.
2. Anticoagulation Medication
- What It Is: Commonly known as “blood thinners,” these medications prevent new clots from forming and reduce the risk of blockages in the veins.
- When It’s Used: Often, anticoagulants are prescribed after stenting to keep the blood flowing smoothly through your veins.
3. Compression Therapy
- What It Is: Compression stockings apply gentle pressure to your legs, which can help reduce swelling and improve blood flow.
- How It Helps: Compression is often used with other treatments and can help ease symptoms like pain and swelling.
Why Follow-Up Care is Important
If you have a stent placed, follow-up care is essential to keep it working well. Your doctor might recommend:
- Regular imaging tests to check that the stent is staying open
- Continued medication to prevent clots from forming in the stent
- Healthy habits, like staying active and wearing compression stockings if recommended
What Can I Do to Manage PTS?
Luckily, there are steps you can take to keep PTS in check. Here are some tips:
- Wear Compression Stockings
Compression stockings improve blood flow and can reduce swelling and pain. Your doctor may recommend wearing them daily, especially if you’re on your feet a lot. - Stay Active
Walking, swimming, or light exercise helps with circulation. Moving regularly prevents blood from pooling in your legs. - Elevate Your Legs
When resting, prop your legs up on pillows to help reduce swelling. - Skincare Matters
Use moisturizers to keep your skin healthy and prevent itching or breakdown. If you develop any sores, let your doctor know right away.
Final Thoughts: You Don’t Have to Live with Post-Thrombotic Symptoms!
Living with post-thrombotic venous occlusion can be challenging, but treatments like stenting, medication, and compression therapy offer real hope for relief. By working closely with your doctor and following your treatment plan, you can manage your symptoms and get back to doing the things you love.