If you’re experiencing ongoing pelvic pain, you’re not alone. Chronic pelvic pain affects many people, especially women, and can significantly impact your day-to-day life. The good news? By understanding the causes and treatment options, you can take steps toward finding relief.
What is Chronic Pelvic Pain?
Chronic pelvic pain is discomfort in the lower abdomen that lasts for six months or longer. It can come and go, or be constant, and may vary in intensity. Common symptoms include:
- Pain during or after sex (dyspareunia)
- Painful menstrual periods (dysmenorrhea)
- Lower back pain
- Abdominal pain
This type of pain can significantly affect your quality of life, making it important to understand the potential causes and treatment options.
What Causes Chronic Pelvic Pain?
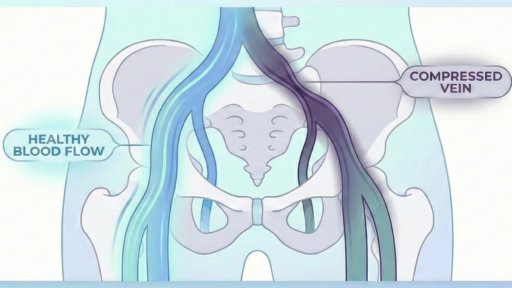
There are several reasons why you might be experiencing chronic pelvic pain, including issues with the veins in your pelvis. One of the most common causes is pelvic venous disorders, which happen when the veins in the pelvic area become enlarged and don’t function properly. Venous causes of pelvic pain are due to:
- Reflux: where blood flows in the wrong direction and pools in the veins, causing them to enlarge and create pressure and pain.
- Obstruction: when veins are compressed by surrounding structures, leading to restricted blood flow and discomfort.
Other possible causes of chronic pelvic pain include:
- Endometriosis: when tissue similar to the lining inside the uterus grows outside of it, leading to pain, especially during menstruation.
- Fibromyalgia: a condition that causes widespread pain, including in the pelvic region.
- Nerve entrapment: when nerves in the pelvis become compressed, leading to pain.
How Are Pelvic Vein Problems Diagnosed?
If your doctor suspects a problem with your pelvic veins, they may recommend imaging tests, such as ultrasound or MRI scans, to get a closer look at what’s happening inside your body. Ultrasound, in particular, is a great tool for seeing if there are any problems with your veins, such as compression or blood pooling.
By diagnosing these conditions early, your doctor can help create a personalized treatment plan that will give you the best chance of relief.
What Are the Treatment Options?
Not everyone with pelvic vein issues needs treatment. In fact, many people with pelvic venous incompetency (when the veins don’t work properly) have no symptoms at all.
However, if your pelvic pain is linked to a vein problem, your doctor might suggest treatments such as:
- Medication to manage pain and inflammation.
- Minimally invasive procedures like embolization, which involves blocking off the problematic veins to stop blood from pooling.
- Surgery in more severe cases.
These treatments are generally very effective and can significantly improve symptoms in most people.
Living with Chronic Pelvic Pain
Living with chronic pelvic pain can be challenging, but there are ways to manage it. Working with a team of healthcare providers—including doctors, physical therapists, and mental health professionals—can help you find the right combination of treatments to improve your quality of life.
If you’re struggling with pelvic pain, talk to your doctor about what you’re experiencing. With the right diagnosis and treatment, relief is possible!